Menu
Sample Required: Blood | Test Type: Genetic
Key Advantages
DNA Pain is a genetic test that offers insight into key biological pathways that influence chronic pain and comorbid conditions, offering personalised diet, nutraceutical, exercise and lifestyle recommendations for improved chronic pain management.
Genes are segments of DNA that contain the instructions your body needs to make each of the many thousands of proteins required for life. Each gene is comprised of thousands of combinations of “letters” (called bases) which make up your genetic code. The code gives the instructions to make the proteins required for proper development and function.
Genetic variations (small differences in our DNA) can affect the expression of a gene, thereby affecting metabolic processes that are important for maintaining cellular health and how we respond to environmental interventions such as diet, lifestyle, supplements, and medication. Knowledge of these genetic variations offers unparalleled insight into your biological systems, allowing your healthcare practitioner to recommend precise interventions aimed at helping you reach your goals and achieve optimal health.
Chronic pain is defined as any persistent or intermittent pain that lasts more than 3 months. Whilst injury or a disease may be the primary cause of chronic pain, only a small minority of those subjected to injury develop chronic pain. Research shows that chronic pain is highly heritable, meaning there is a strong genetic component.
This report tests for genetic variations associated with changes in key biological pathways known to modulate susceptibility to chronic pain. Weaknesses in these pathways, together with environmental factors, can increase risk for the development of chronic pain. This report provides valuable insights into
individual priority areas that should be considered for successful and sustained chronic pain management
outcomes with a focus on personalised diet, nutraceutical, exercise, and lifestyle interventions.
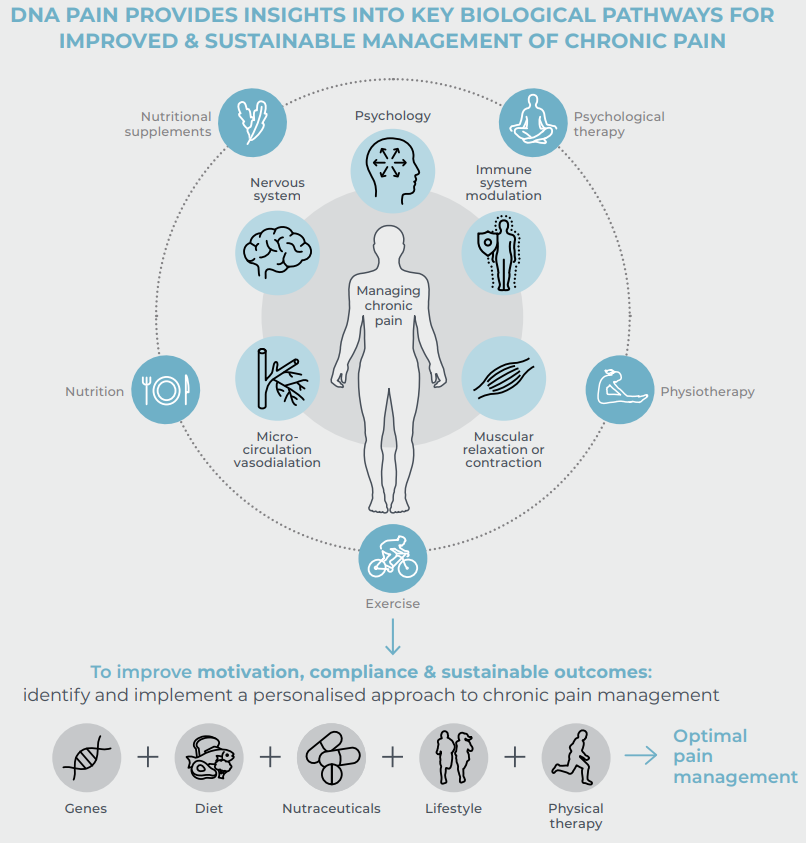
Chronic pain affects 1 in 5 people globally and features prominently in the top 10 causes of disability. It is a complex multifactorial disease that is the result of an interplay between an individual’s environment, lifestyle, and genetic makeup which influence the duration, intensity, perception and effects (physical, psychological, social & emotional) of chronic pain. Evidence shows that genetic variants associated with chronic pain can influence the function of various biological pathways. In addition, those suffering from chronic pain are at a higher risk of comorbid conditions such as anxiety or depression which can exacerbate pain perception because of their shared biological pathways and overlapping pathophysiology.
Current chronic pain management treatments are associated with negative side-effects and display variable effectiveness at the population level (attributed to interindividual variability in pharmacokinetic and pharmacodynamic properties of analgesic medications). Evidence-based non-pharmacological treatment approaches including nutritional/dietary modification, physical training exercises, and cognitive & behavioural mind/body techniques are now becoming more widely used. These approaches have improved morbidity and function in patients with chronic pain, and simultaneously reduced the risks and impact of common comorbidities. They also have reduced risk of adverse events and addiction liability. The knowledge gained from this test supports the implementation of a holistic and personalised
approach to managing chronic pain.
Mon – Fri 8am to 5.00pm NZT
orders@fxmed.co.nz
support@fxmed.co.nz
NZ customers
Free Phone: 0800 439 633
Free Fax: 0800 439 630
Australian customers
Free Phone: 1800 770 904
Free Fax: 1800 665 070

Please note that all products and services found on this website are available to patients through their health practitioner only.
New to FxMed? Set up your account and access leading brands trusted by practitioners in Australia and New Zealand.